WHY ‘HERD IMMUNITY’ ISN’T AS SIMPLE AS ‘HERDING’ — AN INDIA CASE STUDY
Ranju Anthony
While this article is being written, Covid-19 is spreading further in India, with an increased risk of spiraling into a community transmission mode. As on July 14, the case load looks pretty high at 900,000 (or 9 lakh) plus cases, the relief, however, comes across through higher recoveries, which is at a healthy 63% or 5.72 lakhs recovered cases & a still relatively low crude fatality rate of 2.61% (23,727 deaths). Now, to live with Covid-19, and that could be practically for a good many months from now, many medical practitioners, academicians & even politicians have advocated for a dire need of experimenting with a concept called ‘Herd Immunity’, which is also known as ‘Community Immunity’.
The literal meaning of ‘Herd Immunity’ & its association with ‘Vaccines’
Herd immunity in a population occurs when an adequate number of individuals attain immunity to a specific disease, thus, protecting the remaining lesser immune of the population. By sheer definition, ‘Herd immunity’ is the ‘resistance of a group to attack by a disease to which a large proportion of the members are immune, thus lessening the likelihood of a patient with a disease coming into contact with a susceptible individual’ (Fox et al., 1971). Which in plain speak means, that an ‘immune person’ has the ability to ‘break the chain of infectivity’ & the more the number immune individuals in a chain, the more, the likelihood of the said infection to get eradicated from a population. It is imperative to note though that ‘herd immunity threshold’ varies among different infectious diseases, plainly due to the fact that the associated risk of transmission also differs from disease to disease. For example, the transmission dynamics of HIV completely differs from say, transmission of Covid-19 or even plain influenza in a population.
Now how do an individual attain ‘immunity’ from a disease? The simplest answer is, by being administered a ‘Vaccine’. For a community wide control of an epidemic (or a pandemic like ‘Covid-19’), the first & the most essential step is development of a safe, efficacious & cheap vaccine that can be scaled up easily to large population tracts. Technically, a vaccine is a reservoir of agents constructed from a weakened form of micro-organisms that stimulates production of antibodies that trigger immune systems in a human body.So ideally, ‘Herd Immunity’ as a concept should ONLY be propagated or conceptualized while a vaccine is absolutely ready for the mentioned population’. In fact, the concept of ‘Herd Immunity’ in itself is as an extension of the protection imparted by an immunization program beyond the vaccinated to the unvaccinated individuals (Fine, 1993). Apart from vaccines, though, another commonly heard interpretation about ‘herd immunity’ is that the transmission of any subject virus can be controlled through mass infection.
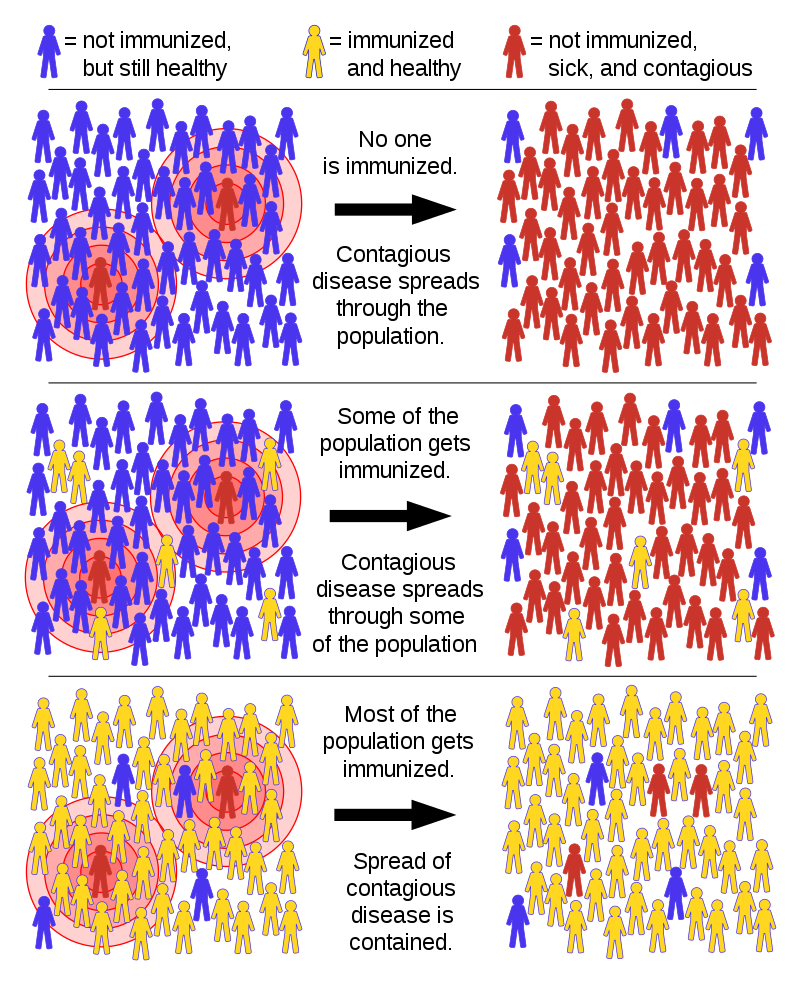
Image Source: Image: Tkarcher / CC BY-SA
Now before we go any further, it is important to also try & understand as to how a progression of an infectious disease is tracked in a population.
Basic Reproductive Rate R0 Simplified
Progression of an infectious disease or its transmission potential is tracked through a metric known as ‘basic reproductive rate’ or R0 (or R ‘naught’). ‘R0’ is an average number of secondary cases produced by one primary case in a wholly susceptible population (Anderson et al. 1985). ‘Susceptible population’ is essentially a population that has not been ‘immunized’ and is yet to contact a contagious disease like Covid-19. The reproductive rate of a disease is categorized in values starting from 0 to any higher number, usually in decimal points.
In the case of Covid-19, as in second week of July, India, has an R value of 1.11, albeit, cities like Delhi are witnessing a much higher reproductive rates, fluctuating between, 1.20 to 1.41. In retrospect, what it means is, in Delhi, say, going by its R0 value of 1.41, 1000 active cases of Covid-19 have the potential to further infect 1410 healthy people. Which means, by the end of Day 30, these originally 1000 active cases would get converted into 29962178 or almost 3 million active cases.
Now to further explain the importance of these decimal units, let’s try using the national R0 value of 1.11 on the same number of 1000 active cases, which translates to 1110 cases in the second generation can lead to a case load of 22892 cases by the end of Day 30, a difference of more than 2.99 million cases with just a seemingly small difference of (1.41–1.11 = 0.30 Units).
So what happens when the value of R0 equals to 1 or less than 1? In a case where R0=1, or rather, when it is presumed that 1 active case have a potential to infect 1 healthy person, an epidemic’s level reaches a ‘stable’ point from where the chances of another major escalation of cases are far less. However, if the R0 value<1 then the disease is expected to decline & eventually elapse with sustained follow-up on the population by the legislature, through sustained surveillance mechanisms. The whole concept of R0 only gets applied; when it’s proven that the infectious disease is a ‘novel disease’ with no vaccines or control interventions in place.
Herd Immunity in Action & Importance of Vaccine Development
Now with a presumption that a vaccine is indeed ready & has already been shipped into the country, the hidden numbers may be triangulated. Since, the last census happened in 2011, let’s take into account, the United Nation’s data for India’ population in 2020, i.e. 1.38 Billion (World Bank Estimation). Going back to India’s R0; the national reproductive value for Covid-19 presently stands at 1.11. For India, the critical vaccination rate in percentage that is denoted by ‘Qc’ may be computed as; Qc= (1–1/1.11)*100 or 0.10*100, or 10% for the whole population of India, which in turn equals to 138 million individuals. In other words, for India to achieve ‘Herd Immunity’, 138 million of the population needs to be completely vaccinated / immune to Covid-19.
Now, in the absence of a vaccine, if we were to ‘allow’ the entire population of 1.38 billion to move around freely & contribute to this ‘immune’ number of 138 million, the end result would translate to hospitalizations & fatalities of catastrophic propositions. India’s case fatality rate at the moment is less than 3% (precisely 2.61%). Presuming that the CFR remains constant, the minimum fatalities that India would encounter would be approximately 32 million casualties. Now, let’s also talk about a slightly greater fatality rate worth 5% and the fatality number balloons to 62 million deaths, and this may not be the worst, keeping in view of the health system infrastructure of our country. Notwithstanding, that the country would be magnanimous enough to withstand these appalling fatality rates since the majority of the brunt would be borne by a particular section of a population, the associated risks outweigh any such misadventure.
Moreover, as in other countries, the transmission of Covid-19 in our population is not ‘homogenous’, which means, that to have a more definitive theory in terms of how Covid-19 transmits in a population, exploratory research studies focused on heterogeneity in transmission needs to be further captured, including, as to how ‘Covid-19’ reacts with heterogeneous factors like human genetics, different age groups, different health behavioral tenets & geographical distribution of hosts. These important factors also hold well for ‘acquiring’ immunity against Covid-19, or for cases that we keep hearing as ‘asymptomatic cases’, wherein an individual body’s inherent immunity is able to fight & neutralize the progression of this disease. Only after documenting ample research outcomes, can a country, as large as India, can even think about implementation of control models such as ‘herd immunity’.
Vaccine development involves a painstakingly innovation process that involves many a sub-processes, encompassing different development partners, including, biomedical scientists, clinical development professionals, regulatory bodies, manufacturing organizations & most importantly, a government or an internationally funded global body that authenticates or embodies a vaccine’s quality & quality control mechanisms in place. Presuming that all the countries are focused & channeling all their resources in tandem for one of the most important vaccines in recent times, a (credible) vaccine for Covid-19 is still at least 10–15 months away from landing onto our palms. This practically means that preventive strategies & their successful implementation would remain the focal point for containing this novel coronavirus for a considerable period.
References
- Anderson, R. M., & May, R. M. (1985). Vaccination and herd immunity to infectious diseases. Nature, 318(6044), 323–329. doi:10.1038/318323a0
- Fox J.P. et al. (1971). Herd Immunity: Basic Concept & Relevance to Public Health Immunization Practices. American Journal of Epidemiology, Vol. 94, №3, PP. 179–189.
- Fine P.E.M. (1993). Herd Immunity: History, Theory, Practice. Epidemiologic Reviews, The John Hopkins University School of Hygiene and Public Health, Vol. 15, №2, PP. 265–302.
- Population Estimates and Projections, Data Catalog. The World Bank https://datacatalog.worldbank.org/dataset/population-estimates-and-projections)
ABOUT US
Transdisciplinary Research Foundation or TRF is a Section VIII non profit research focused organisation.
ALL CONTACTS
- C-9/9867, Vasant Kunj, New Delhi-110 070
- Office +91 9910487009
- ranju@tresfoundation.org
- Tresfoundation - Copyright 2021
- ranju@tresfoundation.org